Connect With Us
Blogs

Can Morton's Neuroma Go Away?

Morton’s neuroma, known as intermetatarsal neuroma, is an inflamed nerve in the ball of the foot, typically behind the third and fourth toes. It can occur from wearing tight shoes or from having foot deformities. Morton’s neuroma presents itself as pain, swelling, numbness, tingling, or burning of the front of the foot. Those who have had this condition liken it to the feeling of walking on a pebble or rolled-up sock. This nerve is sensitive to excessive weight on the foot and scar tissue can form around the nerve and sometimes enlarge it. Those who wear high heels or tight-fitting shoes are susceptible to this condition. Treatments vary by the severity of Morton's neuroma. Resting the foot, cushioning the ball of the foot with padding, and wearing orthotics to take pressure off of the nerve can help. If more conservative treatment does not relieve discomfort, surgery can be performed to remove the inflamed nerve segment. If you are suffering from pain in your midfoot, it is suggested that you make an appointment with a podiatrist for a proper diagnosis and a treatment plan that is customized to your situation.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Jeffrey L. Bober, DPM of Maryland. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
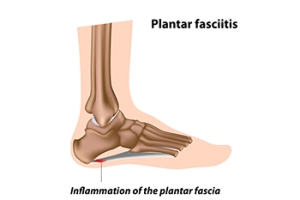
Plantar Fasciitis and Toe Extensions
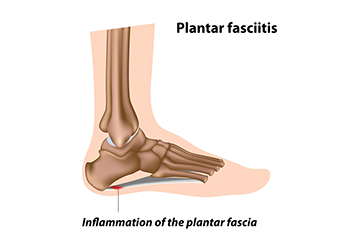 Plantar fasciitis is one of the leading foot conditions among Americans causing heel pain. The condition is characterized by the aggravation of the plantar fascia. Depending on your particular case of plantar fasciitis, a medical professional might recommend that you perform any number of stretches to mitigate the pain. For example, a medical professional, such as a podiatrist, might recommend that to combat plantar fasciitis, you can perform toe extensions. This stretch can be performed by putting the affected foot behind the other in a standing position. Then, contract the calf muscles and lift the back heel to essentially extend the toes. If you are someone that is living with plantar fasciitis, it is suggested that you contact a podiatrist today for an exam and treatment options.
Plantar fasciitis is one of the leading foot conditions among Americans causing heel pain. The condition is characterized by the aggravation of the plantar fascia. Depending on your particular case of plantar fasciitis, a medical professional might recommend that you perform any number of stretches to mitigate the pain. For example, a medical professional, such as a podiatrist, might recommend that to combat plantar fasciitis, you can perform toe extensions. This stretch can be performed by putting the affected foot behind the other in a standing position. Then, contract the calf muscles and lift the back heel to essentially extend the toes. If you are someone that is living with plantar fasciitis, it is suggested that you contact a podiatrist today for an exam and treatment options.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Jeffrey L. Bober, DPM from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Let the Expert Treat Your Ingrown Toenails
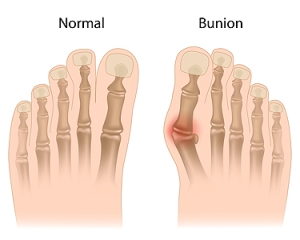
Various Types of Bunions

Research has shown that bunions are the most common medical condition that affects the front of the foot. It is easy to notice by the large bump that develops and protrudes on the side of the big toe. Severe bunions may cause the other toes to shift together, and larger shoes may need to be purchased. A bunion is considered to be a deformity and can happen from wearing shoes that do not have ample room for the toes to move freely in. High heels can fit into this category, and it is helpful to limit how frequently they are worn. There are various types of bunions, and a simple bunion is a bump on the side of the big toe joint. The same bunion may have skin irritation from rubbing against the shoes and a tailor’s bunion forms on the pinky toe. Bunions with hallux limitus can change the structure of the foot, which may cause the bunion to form on the top instead of on the side of the foot. Some people can help to wear a protective pad over the bunion for mild relief. If you have a bunion, it is strongly suggested that you visit a podiatrist who can offer you treatment options that are correct for you.
If you are suffering from bunion pain, contact Jeffrey L. Bober, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Various Types of Orthotics

Orthotics are inserts that are put inside the shoes which can help to correct problematic foot structures. People who have flat feet, high arches, or foot conditions such as arthritis and plantar fasciitis may benefit from wearing orthotics. Soft, rigid, and semi-rigid are the different types of orthotics to choose from, and each kind is designed to provide the desired results for the specific foot condition. Soft orthotics may provide cushioning that can help to absorb shock, in addition to reducing pressure while walking. Plastic or graphite materials are used to make rigid orthotics, which and may help to improve alignment and movement. The most common types of orthotics are semi-rigid and are constructed with flexible materials that lie over a firm bottom layer. People who have diabetes may wear orthotics as a method of preventing sores or blisters from developing. If you would like to have more knowledge about orthotics, it is suggested that you confer with a podiatrist who can provide you with the information you are seeking.
If you are having discomfort in your feet and would like to try orthotics, contact Jeffrey L. Bober, DPM from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Two Groups of Foot Muscles

People who frequently go to the gym understand the importance of exercising the muscles in their bodies. With this being noted, the feet are often neglected, and many people fail to properly stretch and exercise their feet. The muscles in the feet can be categorized into two different areas, and the intrinsic foot muscles can be referred to as the core of the feet. The arch is maintained by these muscles and can aid in shock absorption. Global muscles are typically larger, and the ankle is moved by these types of muscles, which are also responsible for pointing and flexing the toes. Common exercises to perform consists of picking up marbles with the toes. This stretch can engage both groups of muscles. A strengthening exercise for the toes can be done by spreading them out as far as possible, repeated several times. If you would like more information about how foot exercises can benefit the feet, it is suggested that you speak with a podiatrist who can guide you toward effective foot stretches to perform.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact Jeffrey L. Bober, DPM from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctor to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.