Connect With Us
Blogs

A Common Treatment Option for a BrokenToe
 Common causes of broken toes can include stubbing your toe against a piece of furniture or dropping a heavy object on it. Each toe consists of small bones and can abruptly break from sudden impact. It can be easy to notice a broken toe: Common symptoms include severe pain, bruising, and swelling. Relief may be found when the affected foot is elevated, and this may help to reduce some of the swelling. Some patients find it helpful to tape the broken toe to the toe next to it. This is referred to as buddy taping and can be effective in providing necessary stability. It is suggested to stay off the foot, and to refrain from physical activity that requires walking. If you have broken your toe, please seek counsel from a podiatrist who can help you with correct treatment methods.
Common causes of broken toes can include stubbing your toe against a piece of furniture or dropping a heavy object on it. Each toe consists of small bones and can abruptly break from sudden impact. It can be easy to notice a broken toe: Common symptoms include severe pain, bruising, and swelling. Relief may be found when the affected foot is elevated, and this may help to reduce some of the swelling. Some patients find it helpful to tape the broken toe to the toe next to it. This is referred to as buddy taping and can be effective in providing necessary stability. It is suggested to stay off the foot, and to refrain from physical activity that requires walking. If you have broken your toe, please seek counsel from a podiatrist who can help you with correct treatment methods.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Jeffrey L. Bober, DPM from Maryland. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Does Your Child Walk On the Outside of One Foot?
The tarsal navicular bone helps connect the ankle to other bones that are lower in the foot. This bone gets its nautical sounding name because it has a shape that is like a small boat. The navicular bone helps form and stabilize the arch and helps us walk efficiently. Kohler’s Disease is a rare bone disorder in which the navicular bone experiences a loss of blood supply and density, causing the bone to weaken and be susceptible to compression from other bones in the foot. This can affect some children typically aged 3-7, and it most commonly occurs in boys. The symptoms a child may experience with Kohler’s Disease include pain, tenderness, swelling, and redness in the middle of the foot. While this disorder may sound scary, the prognosis is usually good: Kohler’s Disease generally corrects itself as the child matures. Until that time, the child may compensate for the discomfort they are feeling by walking on the outside of the affected foot. If you see your child walking like this or even limping, it is wise to take them to a podiatrist for an examination and diagnosis. If their findings indicate that your child has Kohler’s Disease, the podiatrist can help treat the disorder and provide relief through techniques such as casting, anti-inflammatory medications, custom orthotics and special supportive footwear.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact Jeffrey L. Bober, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Child's Feet
It is never normal for a child to experience pain in his or her feet. Foot pain that lasts more than a few days and limits a child’s ability to walk should be examined by a podiatrist. Many adult foot ailments originate in childhood and may be present at birth. Common foot issues that are experienced by children are pediatric flat foot, Sever’s disease, ingrown toenails, and plantar warts.
A child’s foot grows rapidly during the first year, allowing it to reach almost half of their adult foot size. Consequently, foot specialists consider the first year to be the most crucial point in the foot development process. There are ways you can help ensure that your child’s foot develops properly. One way is to carefully look at your baby’s feet. If you notice any deformities, you should immediately seek professional care. You should also loosely cover your child’s foot, since tight coverings may prevent movement and inhibit normal development. Another tip is to change the baby’s positioning throughout the day. If your baby lies down in one spot for too long, it may put an excess amount of strain on the feet and legs.
It is best that you try not to force a child to start walking. Children will begin to walk when they are both physically and emotionally capable to do so. You should also avoid comparing your child’s walking progress with other children because the age range for independent walking may range. When your child’s feet begin to develop, you may need to change both their shoe and sock size every few months to allow room for their feet to grow.
Kids are sometimes prone to splinters, cuts, and severe injuries because they tend to walk around barefoot. This also makes them more susceptible to developing plantar warts which is a condition caused by a virus that invades the sole of the foot through breaks in the skin. These ailments can be avoided by making sure your child wears shoes in unsanitary environments. You should also wash any minor cuts or scrapes on your child’s feet. It is a myth that exposure to fresh air will heal injuries; fresh air will only expose your child’s cuts to germs.
As a parent, you should ensure that your child’s feet are developing properly and are being properly maintained. Consequently, it is important that you perform routine inspections on his or her feet to detect any injuries or deformities in their early stages. Early detection and treatment will help to ensure that your child does not develop any serious foot conditions.
Reasons You Might Have an Ingrown Toenail
 An ingrown toenail occurs when the outer edge of a toenail grows into the surrounding skin, rather than over it. This causes redness, swelling, pain, and inflammation around the ingrown toenail. The area is also at an increased risk of infection. Several factors make an ingrown toenail more likely to develop. Trimming the toenails improperly, by cutting them too short or into a rounded shape, makes the skin more likely to fold over the nail. Wearing shoes that are too tight or narrow in the toe area can squish the nails into the skin. Having excessively sweaty feet can make the skin surrounding the nails too soft, allowing the nail to pierce through the skin more easily. Sometimes an injury to the toenail can cause an ingrown nail to develop. Some people also have nails that naturally grow in a curved or fan-like shape that can make ingrown nails more likely. If you have a painful or infected ingrown toenail, or if you are prone to ingrown toenails, it is suggested that you seek the care of a podiatrist.
An ingrown toenail occurs when the outer edge of a toenail grows into the surrounding skin, rather than over it. This causes redness, swelling, pain, and inflammation around the ingrown toenail. The area is also at an increased risk of infection. Several factors make an ingrown toenail more likely to develop. Trimming the toenails improperly, by cutting them too short or into a rounded shape, makes the skin more likely to fold over the nail. Wearing shoes that are too tight or narrow in the toe area can squish the nails into the skin. Having excessively sweaty feet can make the skin surrounding the nails too soft, allowing the nail to pierce through the skin more easily. Sometimes an injury to the toenail can cause an ingrown nail to develop. Some people also have nails that naturally grow in a curved or fan-like shape that can make ingrown nails more likely. If you have a painful or infected ingrown toenail, or if you are prone to ingrown toenails, it is suggested that you seek the care of a podiatrist.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Jeffrey L. Bober, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Tarsal Tunnel Syndrome and Rheumatoid Arthritis
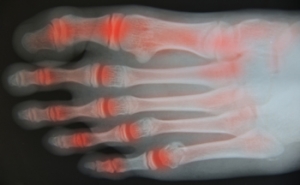
 Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks the otherwise healthy cells that make up the linings of joints. Because each foot contains 33 joints, the feet, as well as the ankles, are often affected. RA can make other foot and ankle conditions more likely to occur. One such condition is tarsal tunnel syndrome, in which the posterior tibial nerve is compressed or damaged, causing burning pain, numbness, and tingling in the affected foot. Tarsal tunnel syndrome is frequently seen in people with RA. If you have RA, it is suggested that you be under the care of a podiatrist who can monitor the health of your feet and treat any problems as they arise.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Jeffrey L. Bober, DPM of Maryland. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
Medications for Fungal Toenail Infections
Toenail fungus is extremely common, affecting about 5.5% of adults around the world. This condition can cause the toenails to become brittle, crumbly, discolored, or misshapen. In severe cases, the nails may even begin to separate from the nail bed and emit a foul odor. Treating fungal toenails can be difficult, as it can take a long time before there are visible results. There are various treatment options available, including topical medications that are applied directly to the nail, oral medications that are taken by mouth, and laser treatment. Currently, many podiatrists prescribe a combination of oral and topical treatments. While these medications can be effective, oral medications may cause unwanted side effects, and topical medications are not as effective for severe infections. If you have toenail fungus, it is suggested that you are under the care of a podiatrist.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Jeffrey L. Bober, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Glen Burnie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.